Understanding the Far-Reaching Risks of Obesity in Men: A Comprehensive Overview
Obesity in men is more than a weight issue — it’s a complex medical condition with far-reaching health risks. From heart disease and liver problems to hormonal and psychological effects, understanding these connections is key to effective prevention and management.

Understanding the Far-Reaching Risks of Obesity in Men: A Comprehensive Overview
Obesity is far more than just a matter of weight; it’s a complex medical condition with extensive consequences for men’s health. The ongoing obesity epidemic has led to a dramatic rise in obesity-related health issues, driving up rates of metabolic syndrome and cardiovascular conditions. Excess weight, particularly visceral fat accumulation, and associated hormonal imbalances, can significantly increase the risk of a variety of serious health problems. The global burden of obesity continues to rise [1], placing immense strain on health systems and contributing to increased mortality worldwide. This article provides a comprehensive overview of these risks, emphasising the interconnected nature of obesity-related complications.
Obesity and Its Underlying Risks
Obesity is a complex and multifaceted condition characterised by the accumulation of excess body fat, which can significantly increase the risk of chronic diseases such as cardiovascular disease, type 2 diabetes and certain cancers [1]. The development of obesity is influenced by a combination of genetic, environmental and lifestyle factors including unhealthy dietary patterns, lack of physical activity and socioeconomic status. Key risk factors such as hypertension, metabolic syndrome and insulin resistance often accompany obesity [2,3], further elevating the risk of cardiovascular disease and other serious health problems. Understanding these underlying causes is essential for effective prevention and management, as obesity not only impacts physical health but contributes to a wide range of chronic diseases and associated issues.
Measuring and Assessing Obesity
Accurately measuring and assessing obesity is essential to identify individuals at risk of obesity-related health problems. The most commonly used tool is the Body Mass Index (BMI), calculated by dividing a person’s weight in kilograms by the square of their height in metres. BMI categories help classify individuals as underweight, normal weight, overweight or obese, providing a general indication of health risks associated with excess body fat [1,2]. However, BMI does not distinguish between fat and muscle mass, so it may not fully reflect an individual’s health status. Additional measurements, such as waist circumference and waist-to-hip ratio, offer valuable insight into body fat distribution. In men, a waist circumference greater than 102 cm is associated with a higher risk of chronic diseases, including cardiovascular disease and type 2 diabetes [2,3]. By combining these assessment tools, healthcare professionals can better evaluate health risks and tailor interventions to address obesity and its related health problems.
Cardiovascular Disease, Complications, and Metabolic Syndrome
As previously discussed, obesity, especially visceral fat and abdominal obesity, disrupts the body’s ability to regulate blood pressure, blood sugar and lipids, leading to metabolic syndrome [2,3]. Metabolic syndrome includes components such as elevated Triglycerides and low HDL cholesterol, both of which increase cardiovascular risk. This dangerous cluster of risk factors significantly increases the likelihood of:
- Coronary Artery Disease (CAD): Obesity promotes atherosclerosis, the buildup of plaque in the arteries, leading to angina, heart attack and sudden cardiac death [4].
- Stroke: Obesity increases the risk of both ischaemic and haemorrhagic strokes. Ischaemic strokes occur when blood flow to the brain is blocked; haemorrhagic strokes happen when a blood vessel in the brain ruptures [5].
- Heart Failure: Obesity strains the heart muscle, eventually causing the heart to fail in pumping sufficient blood to meet the body’s needs [6].
- Type 2 Diabetes: Obesity is a major risk factor for type 2 diabetes, a chronic condition in which the body fails to regulate blood sugar properly [2].
Men with obesity are at high risk for adverse cardiovascular outcomes including ischaemic heart disease, myocardial infarction, coronary heart disease, peripheral vascular disease, cerebrovascular disease and cardiovascular mortality [7].
Abdominal obesity and excess fat are key cardiovascular risk factors that can increase blood pressure and contribute to associated pathologies . The presence of other risk factors, such as high blood glucose and high blood cholesterol, further elevates cardiovascular risk. Statistical analysis of large cohorts has demonstrated the impact of these risk factors on cardiovascular outcomes. [3,4]
Men tend to develop these conditions earlier and more aggressively than women [7].
Fatty Liver Disease (MASLD and MASH)
Obesity is a leading cause of Metabolic dysfunction-Associated Steatotic Liver Disease (MASLD) where fat accumulates in the liver and MASH (Metabolic dysfunction-Associated Steato Hepatitis). In MASH, fat accumulation in the liver leads to inflammation and liver cell injury, and sometimes fibrosis (scarring). Reducing body weight by even a modest percentage, such as 3–7 %, can significantly decrease liver fat and improve liver function [8]. MASLD can progress to more severe liver conditions, including:
- MASH: A more severe form of fatty liver, characterised by inflammation and liver cell damage [8].
- Cirrhosis: A late-stage liver disease in which healthy liver tissue is replaced by scar tissue [8].
- Liver Failure: When the liver is no longer able to perform its essential functions [8].
- Hepatocellular Carcinoma (Liver Cancer): MASLD and MASH increases the risk of developing liver cancer [9].
Lifestyle changes in the early stages of fatty liver disease are crucial for slowing disease progression and preserving liver function [8,9].
Sarcopenic Obesity and Excess Body Fat
In aging men, obesity can combine with age-related muscle loss, a condition known as sarcopenic obesity. This combination is particularly dangerous, as it increases the risk of [10]:
- Frailty: Sarcopenic obesity leads to a decline in physical function and an increased vulnerability to stressors.
- Falls: Loss of muscle mass and strength increases the risk of falls, which can lead to fractures and other injuries.
- Disability: Sarcopenic obesity can lead to difficulty performing activities of daily living, such as walking, bathing, and dressing.
- Insulin Resistance: The combination of obesity and muscle loss worsens insulin resistance, increasing the risk of type 2 diabetes.
- Mortality: Sarcopenic obesity is associated with an increased risk of death
Increased Cancer Risk
According to the World Health Organization (WHO), being overweight or having obesity is clearly associated with a higher risk of developing 13 different types of cancer: [1,11]
- Breast Cancer: Cancer of the breast tissue, mainly in women after menopause.
- Ovarian Cancer: Cancer in the ovaries, often hormone-related and linked to higher estrogen levels.
- Thyroid Cancer: Cancer in the thyroid gland in the front of the neck.
- Colorectal Cancer (Bowel or Colon Cancer): Cancer of the large intestine or rectum.
- Gall Bladder Cancer: Cancer in the Gallbladder or Bile ducts, the tubes that connect the liver, gallbladder, and small intestine.
- Pancreatic Cancer: A highly aggressive cancer in the pancreas.
- Meningioma (Brain-covering tumour): Usually benign tumour arising from the membranes covering the brain or spinal cord.
- Multiple Myeloma (Bone-Marrow Cancer): Cancer of plasma cells that produce antibodies.
- Liver Cancer (Hepatocellular Carcinoma): Cancer of the liver, often developing after fatty-liver disease (MASLD/MASH).
- Gastric Cardia Cancer (Upper-Stomach Cancer): Cancer where the stomach joins the oesophagus.
- Kidney (Renal Cell) Cancer: Cancer of the cells inside the kidneys.
- Oesophagus Cancer: Cancer of the oesophagus (food pipe), especially at its lower end.
- Endometrial Cancer (Uterine/Womb-Lining Cancer): Cancer of the uterine lining, strongly linked to obesity and high estrogen levels.
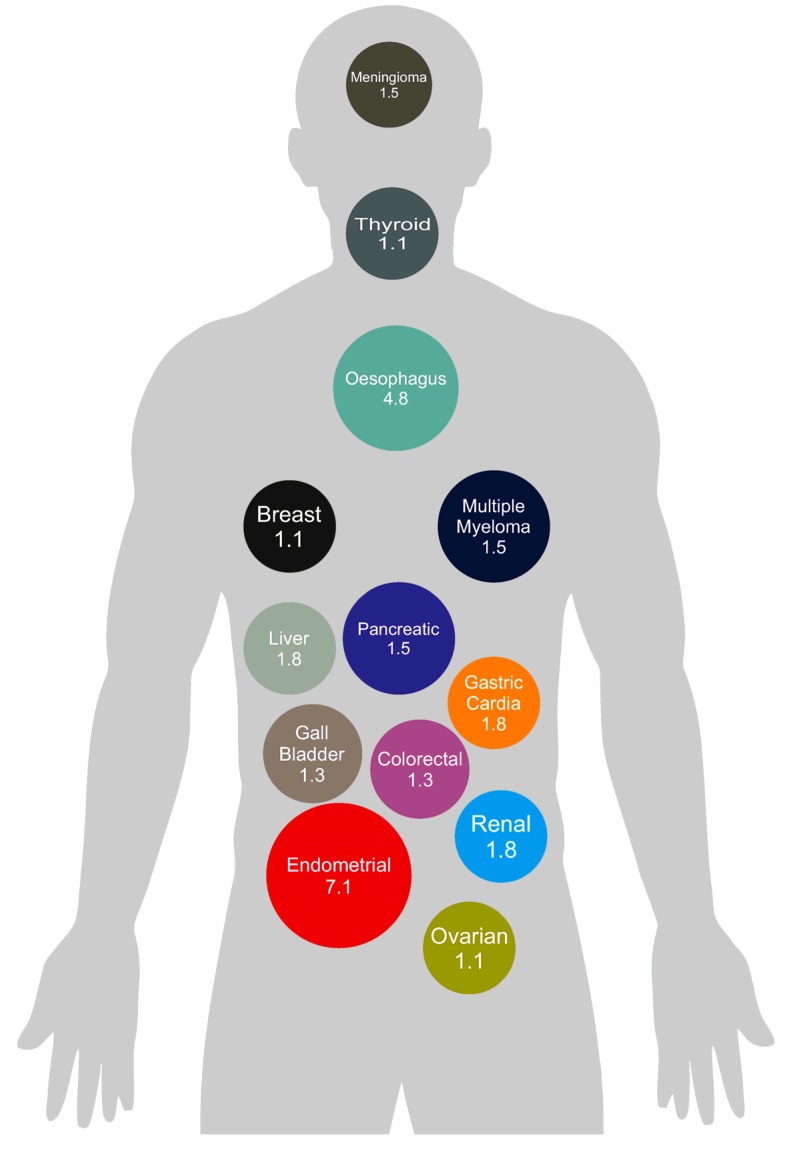
The numbers represent the relative risk (RR) — how many times higher the risk is in people with obesity compared with those of normal weight. There is a 7.1 times higher risk for Endometrial Cancers, 4.8 times higher risk for Oesophageal Cancers and for most other Cancers the risk is 1.3–1.8 times higher when living with obesity than with normal weight [11].
Chronic low-grade inflammation, altered insulin signaling, and hormonal imbalances associated with obesity are thought to contribute to this increased cancer risk.
Low Testosterone Levels (Hypogonadism)
Many overweight and obese men experience low testosterone levels (hypogonadism). Low testosterone can lead to: [12]
- Reduced Libido: Hypogonadism can decrease sexual desire.
- Erectile Dysfunction: Low testosterone can contribute to difficulties achieving and maintaining an erection.
- Infertility: Low testosterone can impair sperm production, leading to infertility.
- Decreased Muscle Mass: Testosterone is essential for maintaining muscle mass; low levels can lead to muscle loss.
- Increased Fat Mass: Low testosterone can promote fat storage, particularly abdominal fat.
- Osteoporosis: Testosterone plays a role in bone health; low levels can increase the risk of osteoporosis.
- Reduced Energy and Motivation: Hypogonadism can lead to fatigue and a decrease in motivation.
The hormonal imbalance also results from increased aromatase activity in fat tissue, converting testosterone into estrogen, leading to elevated estrogen levels and the development of breast tissue (gynecomastia).
Psychological and Societal Factors
The psychological and societal factors associated with obesity can further exacerbate health risks. These factors can significantly impact a man’s mental and emotional well-being, making weight management even more challenging. These include:
- Anxiety and Depression: Obesity is linked to higher rates of anxiety and depression, creating a significant burden on mental health [13].
- Social Stigma: Overweight and obese men may face societal stigma and discrimination, leading to feelings of isolation and a reluctance to seek help. This can negatively impact self-esteem and social interactions [14].
- Unhealthy Coping Mechanisms: In response to psychological distress, some men may turn to unhealthy coping mechanisms, such as excessive alcohol consumption or eating disorders. These behaviors can further worsen both physical and mental health.
- Reduced Mobility: Obesity can limit participation in physical activities, which further impacts both mental and physical health and reduces overall quality of life.
These factors can negatively impact mental and physical health, creating a vicious cycle that makes weight management even more difficult. Addressing these issues requires a compassionate and supportive approach. Additionally, quitting smoking, alongside weight management, can significantly reduce health risks and improve overall well-being.
Pain and Digestive Issues
Excess weight puts increased strain on weight-bearing joints and internal organs, leading to pain and inflammation. Obesity is also associated with an increased risk of digestive issues, significantly impacting quality of life. These include:
- Osteoarthritis: Excess weight accelerates the wear and tear on joints, increasing the risk of osteoarthritis, particularly in the knees and hips. This can lead to chronic pain and reduced mobility [15]. Some men may gain weight due to underlying health conditions or medications, which can further worsen joint pain.
- Gastroesophageal Reflux Disease (GERD): Obesity increases pressure on the stomach, leading to acid reflux and heartburn. Chronic GERD can damage the esophagus and significantly impact quality of life [12].
- Gallstones: Obesity increases the risk of gallstones, which can cause abdominal pain and digestive discomfort, often requiring medical intervention [17].
These conditions can cause chronic pain and discomfort, significantly reducing a man’s ability to engage in physical activity and enjoy daily life. Management often involves weight loss, dietary changes, and medical treatment. Efforts to lose weight can help reduce pain and improve digestive health.
Vitamin D Deficiency
Low vitamin D levels are common in obese individuals due to its storage in adipose tissue, reduced outdoor activity, and potentially altered vitamin D metabolism [18]. Vitamin D deficiency can contribute to:
- Bone Loss and Osteoporosis: Vitamin D is essential for calcium absorption, which is crucial for bone health. Low vitamin D levels increase the risk of bone loss and osteoporosis, increasing fracture risk [17].
- Muscle Weakness: Vitamin D plays a role in muscle function, and deficiency can lead to muscle weakness, increasing the risk of falls and mobility issues [17].
- Impaired Immune Function: Adequate vitamin D is important for a healthy immune system, helping the body fight off infections and maintain overall wellness [19].
Addressing vitamin D deficiency through supplementation and increased sun exposure (when appropriate) is an important aspect of overall health management in obese men. Monitoring vitamin D levels and maintaining adequate levels can have significant benefits [19].
Treatment Options
Effective treatment of obesity requires a personalised approach that takes into account an individual’s health status, lifestyle and preferences [13,14]. Obesity management involves a comprehensive strategy that may include lifestyle modifications, pharmacological treatments, and surgical options, tailored to each individual’s needs. Achieving and maintaining a healthy weight often begins with adopting healthy eating habits, increasing intake of fruits, vegetables and whole grains, while reducing processed foods and sugary drinks [8]. Regular physical activity, including both aerobic exercise and strength training, is crucial for weight loss and long-term maintenance [8]. For some individuals, prescription medicines may be recommended to support weight loss, especially when lifestyle changes alone are insufficient [8]. In cases of severe obesity or when other methods have not succeeded, bariatric surgery may be considered to reduce stomach size and calorie intake [8]. Weight loss surgery is a medical option for those with severe obesity and can help improve related health conditions.
Treating obesity often requires a multidisciplinary approach, combining diet, exercise, medications, and surgical interventions under the guidance of health care professionals. It is important to consult a health care professional for safe and effective obesity management and to treat obesity appropriately.
Reducing Health Risks
Reducing the health risks associated with obesity involves a comprehensive strategy combining lifestyle modifications, behavioural changes and, when necessary, medical interventions [8,13,14]. Maintaining a healthy weight via balanced nutrition and regular physical activity is fundamental to lowering the risk of chronic diseases such as cardiovascular disease, type 2 diabetes and certain cancers [1,4,11]. Managing underlying health conditions like high blood pressure, high cholesterol and elevated blood glucose can further decrease the risk of developing serious health problems [4,6]. Effective disease control is crucial for preventing the progression of cardiovascular and metabolic complications associated with obesity and related conditions. Regular health check-ups and monitoring of vital health metrics enable early detection and prompt management of potential issues [4,6]. Primary care plays a key role in providing comprehensive evaluation and longitudinal tracking of obesity-related health risks. By adopting healthy lifestyle habits, staying physically active and seeking guidance from healthcare professionals, individuals can significantly reduce their risk of obesity-related health conditions and improve their overall quality of life [1,13].
A Way Forward: Addressing Obesity with Confidence
Obesity in men presents a wide range of interconnected health risks. From cardiovascular complications and metabolic syndrome to elevated cancer risk and hormonal imbalances, the consequences of excess weight can be profound. Tackling obesity demands a comprehensive and proactive approach centred on lifestyle change, medical interventions and psychological support [6,13]. Yazen recognises the complexity of these challenges and delivers personalised support to help men manage their weight, reduce their risk of obesity-related complications and enhance their overall health and wellbeing.
References
- World Health Organization. Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Batra et al. 2012. The Role of Visceral Fat. Digestive Diseases. 30.1:70–74. https://doi.org/10.1159/000335722
- Lee et al. 2018. Comparison of the association of predicted fat mass, BMI, and other obesity indicators with type 2 diabetes risk. Eur J Epidemiol. 33(11):1073-1085. https://doi.org/10.1007/s10654-018-0433-5
- Benjamin et al. 2019. Heart disease and stroke statistics 2019 update: a report from the American Heart Association. Circulation. 5;139(10):e56-e528. https://doi.org/10.1161/CIR.0000000000000659
- Quiñones-Ossa et al. 2021. Obesity and Stroke: Does the Paradox Apply for Stroke? Neurointervention;16:9-19 https://doi.org/10.5469/neuroint.2020.00108
- Powell-Wiley et al. 2021. American Heart Association Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; Council on Epidemiology and Prevention; and Stroke Council. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 25;143(21):e984-e1010. https://doi.org/10.1161/CIR.0000000000000973
- Lv et al. 2024. Gender differences in all-cause and cardiovascular mortality among US adults: from NHANES 2005–2018. Front. Cardiovasc. Med. 11:1283132. https://doi.org/10.3389/fcvm.2024.1283132
- EASL–EASD–EASO Clinical Practice Guidelines on the management of metabolic dysfunction-associated steatotic liver disease (MASLD). J Hepatol. 81(6):492–542. https://doi.org/10.1016/j.jhep.2024.06.022
- Li et al. 2024. Risk factors for hepatocellular carcinoma: an umbrella review of cohort studies. Frontiers in Oncology, 14:1175301. https://doi.org/10.3389/fonc.2024.1175301
- Wei et al. 2023. Sarcopenic obesity: epidemiology, pathophysiology, cardiovascular disease, mortality, and management. Front. Endocrinol. 14:1185221. https://doi.org/10.3389/fendo.2023.1185221
- Ingram et al. 2025. The Relationship Between Obesity and Cancer: Epidemiology, Pathophysiology, and the Effect of Obesity Treatment on Cancer. Curr. Oncol. 32:362. https://doi.org/10.3390/curroncol32060362
- Muir CA et al. 2025. Approach to the patient: low testosterone concentrations in men with obesity. J Clin Endocrinol Metab. 110(9):e3125-e3130. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12342380/
- Taylor et al. 2013. The impact of obesity on quality of life. Best Pract Res Clin Endocrinol Metab. 27(2):139-46. https://doi.org/10.1016/j.beem.2013.04.004
- Phelan et al. 2015. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 16(4):319-26. https://pmc.ncbi.nlm.nih.gov/articles/PMC4381543/
- Blagojević et al. 2010. Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthritis and Cartilage, 18(1), 24–34. https://www.oarsijournal.com/article/S1063-4584(09)00225-8/fulltext
- Parra-Landazury et al. 2021. Obesity and Gallstones. Visc Med. 37(5):394-402. https://doi.org/10.1159/000515545
- Rizzoli et al. 2014. The role of dietary protein and vitamin D in maintaining musculoskeletal health in postmenopausal women: A consensus statement from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Maturitas. 80(3):337. https://pubmed.ncbi.nlm.nih.gov/25082206/
- Wortsman et al. 2000. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 72(3):690–693. https://pubmed.ncbi.nlm.nih.gov/10966885
- EFSA NDA Panel 2015. Scientific opinion on vitamin D and contribution to the normal function of the immune system: evaluation of a health claim pursuant to Article 14 of Regulation (EC) No 1924/2006. EFSA Journal. 13(7):4182. https://doi.org/10.2903/j.efsa.2015.4182

October 9, 2025
November 28, 2025
Start your weight loss journey with Yazen today
Everything you need to do is to create an account and answer some questions about your health
.svg)
.svg)
More articles
Levothyroxine for weight loss: myths and risks
On social media and blogs, it’s sometimes claimed that levothyroxine can be used for weight loss. For people living with overweight or obesity, it can be confusing to know what’s actually true. This article explains the risks and what may be useful to know about levothyroxine and weight loss.




.svg)

















